SERVICES IN CARDIOLIGY
Diagnostic
Interventional (Non- Surgical)
Surgical
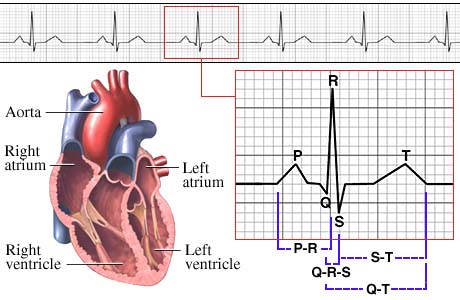
Electrocardiography (ECG)
Electrocardiography is the process of recording the electrical activity of the heart over a period of time using electrodes placed on a patient's body. These electrodes detect the tiny electrical changes on the skin that arise from the heart muscle depolarizing during each heartbeat.
In a conventional 12 lead ECG, ten electrodes are placed on the patient's limbs and on the surface of the chest. The overall magnitude of the heart's electrical potential is then measured from twelve different angles ("leads") and is recorded over a period of time (usually 10 seconds). In this way, the overall magnitude and direction of the heart's electrical depolarization is captured at each moment throughout the cardiac cycle.The graph of voltage versus time produced by this noninvasive medical procedure is referred to as an electrocardiogram (abbreviated ECG or EKG).
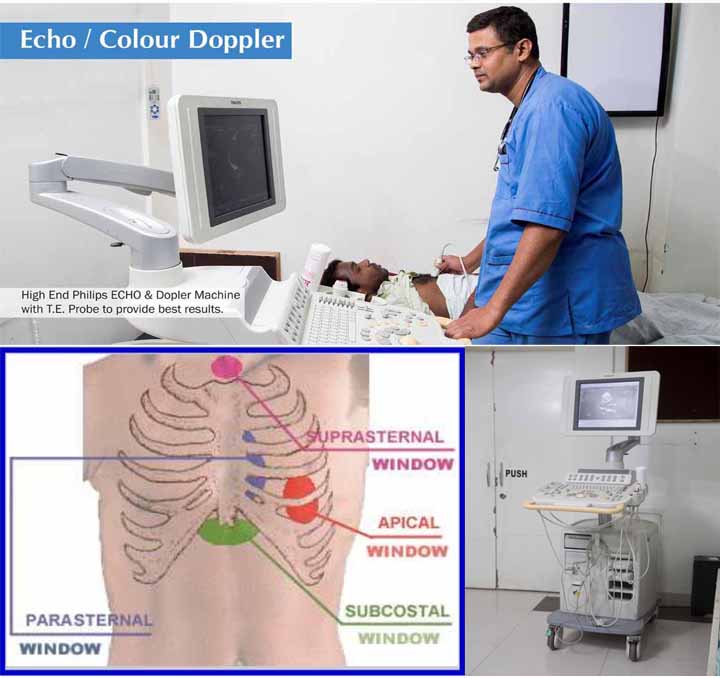
transthoracic echocardiogram (TTE)
A transthoracic echocardiogram (TTE) is the most common type of echocardiogram, which is a still or moving image of the internal parts of the heart using ultrasound. In this case, the probe (or ultrasonic transducer) is placed on the chest or abdomen of the subject to get various views of the heart. It is used for a non-invasive assessment of the overall health of the heart, including a patient's heart valves and degree of heart muscle contraction (an indicator of the ejection fraction). The images are displayed on a monitor for real-time viewing and are also recorded.
An echocardiogram can be used to evaluate all four chambers of the heart. It can determine strength of the heart, the condition of the heart valves, the lining of the heart (the endocardium), and the aorta. It can be used to detect a heart attack, enlargement or hypertrophy of the heart, infiltration of the heart with an abnormal substance. Weakness of the heart, cardiac tumors, and a variety of other findings can be diagnosed with an echocardiogram. With advanced measurements of the movement of the tissue with time (Tissue Doppler), it can measure diastolic function, fluid status, and ventricular dyssynchrony.
transesophageal echocardiogram (TEE)
A transesophageal echocardiogram, or TEE is an alternative way to perform an echocardiogram. A specialized probe containing an ultrasound transducer at its tip is passed into the patient's esophagus. This allows image and Doppler evaluation which can be recorded.
It has several advantages and some disadvantages compared to a transthoracic echocardiogram (TTE).
Specialty medicine professional organizations recommend against using transesophageal echocardiography to detect cardiac sources of embolization after a patient's health care provider has identified a source of embolization and if that person would not change a patient's management as a result of getting more information. Such organizations further recommend that doctors and patients should avoid seeking transesophageal echocardiography only for the sake of protocol-driven testing and to agree to the test only if it is right for the individual patient
dimensional echocardiography (DSE)
3D echocardiography (also known as 4D echocardiography when the picture is moving) is now possible, using a matrix array ultrasound probe and an appropriate processing system. This enables detailed anatomical assessment of cardiac pathology, particularly valvular defects, and cardiomyopathies.[4] The ability to slice the virtual heart in infinite planes in an anatomically appropriate manner and to reconstruct three-dimensional images of anatomic structures make 3D echocardiography unique for the understanding of the congenitally malformed heart. Real Time 3-Dimensional echocardiography can be used to guide the location of bioptomes during right ventricular endomyocardial biopsies, placement of catheter delivered valvular devices, and in many other intraoperative assessments. The 3D Echo Box developed by the European Association of Echocardiography offers a complete review of Three Dimensional Echocardiography.
Three-dimensional echocardiography technology may feature Anatomical Intelligence, or the use of organ modeling technology to automatically identify anatomy based on generic models. All generic models reference a dataset of anatomical information that uniquely adapts to variability in patient anatomy to perform specific tasks. Built on feature recognition and segmentation algorithms, this technology can provide patient-specific three-dimensional modeling of the heart and other aspects of the anatomy including the brain, lungs, liver, kidney, rib cage and vertebra column.
Treadmill testing (TMT)
A cardiac stress test (or cardiac diagnostic test) is a cardiological test that measures a heart's ability to respond to external stress in a controlled clinical environment. The stress response is induced by exercise or by drug stimulation.
Cardiac stress tests compare the coronary circulation while the patient is at rest with the same patient's circulation during maximum physical exertion, showing any abnormal blood flow to the myocardium (heart muscle tissue). The results can be interpreted as a reflection on the general physical condition of the test patient. This test can be used to diagnose coronary artery disease (also known as ischemic heart disease), and for patient prognosis after a myocardial infarction (heart attack).
The cardiac stress test is done with heart stimulation, either by exercise on a treadmill, pedalling a stationary exercise bicycle ergometer, or with intravenous pharmacological stimulation, with the patient connected to an electrocardiogram (ECG). People who cannot use their legs may exercise with a bicycle-like crank that they turn with their arms.
The level of mechanical stress is progressively increased by adjusting the difficulty (steepness of the slope) and speed. The test administrator or attending physician examines the symptoms and blood pressure response. With use of ECG, the test is most commonly called a cardiac stress test, but is known by other names, such as exercise testing, stress testing treadmills, exercise tolerance test, stress test or stress test ECG.
Angioplasty
Angioplasty (or Balloon angioplasty) is an endovascular procedure to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis. An empty, collapsed balloon, known as a balloon catheter, is passed over a wire into the narrowed locations and then inflated to a fixed size. The balloon forces expansion of the stenosis (narrowing) within the vessel and the surrounding muscular wall, opening up the blood vessel for improved flow, and the balloon is then deflated and withdrawn. A stent may or may not be inserted at the time of ballooning to ensure the vessel remains open.
The word is composed of the combining forms of the Greek words. Angioplasty has come to include all manner of vascular interventions that are typically performed in a minimally-invasive or percutaneous method.
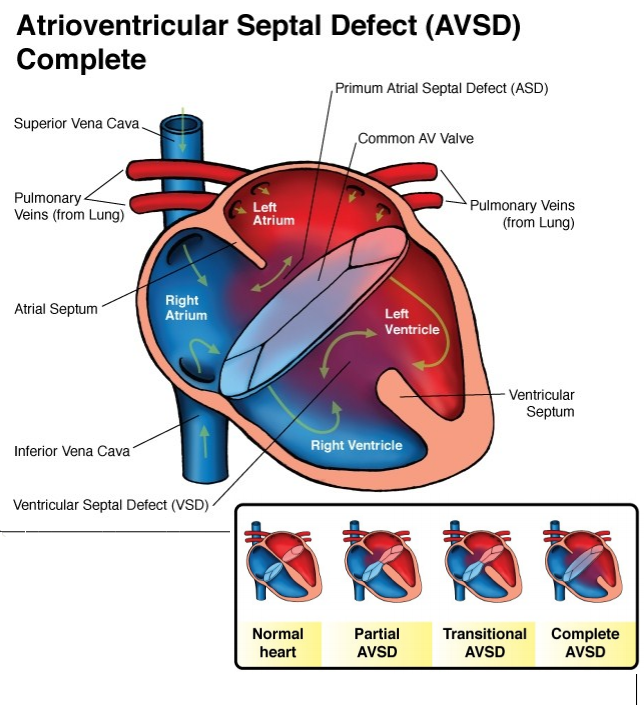
Atrial septal defect (ASD)
Atrial septal defect (ASD) is a congenital heart defect in which blood flows between the atria (upper chambers) of the heart. Normally, the atria are separated by a dividing wall, the interatrial septum. If this septum is defective or absent, then oxygen-rich blood can flow directly from the left side of the heart to mix with the oxygen-poor blood in the right side of the heart, or vice versa.[1] This can lead to lower-than-normal oxygen levels in the arterial blood that supplies the brain, organs, and tissues. However, an ASD may not produce noticeable signs or symptoms, especially if the defect is small.
A "shunt" is the presence of a net flow of blood through the defect, either from left to right or right to left. The amount of shunting present, if any, determines the hemodynamic significance of the ASD. A "right-to-left-shunt" typically poses the more dangerous scenario.
ventricular septal defect (VSD)
A ventricular septal defect (VSD) is a defect in the ventricular septum, the wall dividing the left and right ventricles of the heart.
The ventricular septum consists of an inferior muscular and superior membranous portion and is extensively innervated with conducting cardiomyocytes.
The membranous portion, which is close to the atrioventricular node, is most commonly affected in adults and older children in the United States. It is also the type that will most commonly require surgical intervention, comprising over 80% of cases.
Membranous ventricular septal defects are more common than muscular ventricular septal defects, and are the most common congenital cardiac anomaly.
Patent ductus arteriosus (PDA)
Patent ductus arteriosus (PDA) is a congenital heart defect wherein the ductus arteriosus fails to close after birth.
Early symptoms are uncommon, but in the first year of life include increased 'work of breathing' and poor weight gain. An uncorrected PDA may lead to congestive heart failure with increasing age.
The ductus arteriosus is a fetal blood vessel that closes soon after birth. In a PDA, the vessel does not close and remains "patent" (open), resulting in irregular transmission of blood between the aorta and the pulmonary artery. PDA is common in newborns with persistent respiratory problems such as hypoxia, and has a high occurrence in premature newborns. Premature newborns are more likely to be hypoxic and have PDA due to underdevelopment of the heart and lungs.
A PDA allows a portion of the oxygenated blood from the left heart to flow back to the lungs by flowing from the aorta (which has higher pressure) to the pulmonary artery. If this shunt is substantial, the neonate becomes short of breath: the additional fluid returning to the lungs increases lung pressure, which in turn increases the energy required to inflate the lungs. This uses more calories than normal and often interferes with feeding in infancy. This condition, as a constellation of findings, is called congestive heart failure.
Coronary artery bypass surgery (CABS)
Coronary artery bypass surgery, also known as coronary artery bypass graft surgery, and colloquially heart bypass or bypass surgery, is a surgical procedure consisting of either diverting the left internal thoracic artery to the left anterior descending (LAD) branch of the left main coronary artery; or a harvested great saphenous vein of the leg, attaching the proximal end to the aorta or one of its major branches, and the distal end to immediately beyond a partially obstructed coronary artery (the "target vessel") - usually a 50% to 99% obstruction. The purpose is to restore normal blood flow to that partially obstructed coronary artery. It is performed to relieve angina unsatisfactorily controlled by maximum tolerated anti-ischemic medication, prevent or relieve left ventricular dysfunction, and/or reduce the risk of death. It does not prevent heart attacks. This surgery is usually performed with the heart stopped, necessitating the usage of cardiopulmonary bypass; however, two alternative techniques are also available allowing CABG to be performed on a beating heart either without using the cardiopulmonary bypass deemed as "off-pump" surgery or performing beating surgery using partial assistance of the cardiopulmonary bypass called as "on-pump beating" surgery. The latter gathers the advantages of the on-pump stopped and off-pump while minimizing their respective side-effects.
Minimally Invasive
Minimally-invasive procedures (also known as minimally-invasive surgeries) have been enabled by the advance of various medical technologies. Surgery by definition is invasive and many operations requiring incisions of some size, are referred to as open surgery. Incisions made can sometimes leave large wounds that are painful and take a long time to heal. Minimally-invasive surgery refers to surgical techniques that limit the size of incisions needed and so lessens wound healing time, associated pain and risk of infection. An endovascular aneurysm repair as an example of minimally-invasive surgery is much less invasive in that it involves much smaller incisions, than the corresponding open surgery procedure of open aortic surgery. This minimally-invasive surgery became the most common method of repairing abdominal aortic aneurysms in 2003 in the United States